This article is part of “Innovations In: Sickle Cell Disease,” an editorially independent special report that was produced with financial support from Vertex Pharmaceuticals.
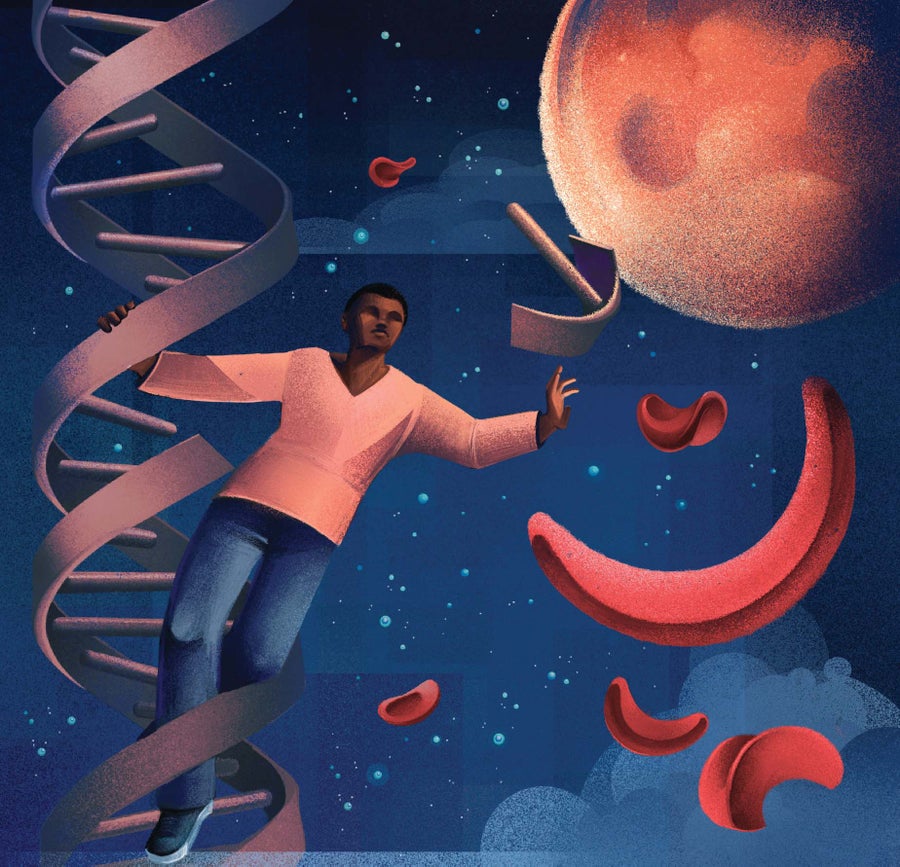
Nathan Wood is 15, lanky and tall. He longs to play basketball; he lives in Yonkers, just outside New York City, and his high school and city parks provide plenty of opportunity for shooting hoops. But his body won’t allow it. Nathan was born with sickle cell disease, an inherited condition that makes round red blood cells collapse into sticky crescents. The distorted cells clump inside blood vessels, depriving tissues of oxygen and inflicting excruciating pain. Exercise or stress or even just changes in routine can trigger a crisis, so Nathan’s mother, Melissa Wood, has often homeschooled him and drives him everywhere—a rare thing in New York, where kids prize their independence.
But the caution is necessary because Nathan’s sickle crises are so frequent. About twice a month, he estimates, he feels the first throbs in his hands or joints, signaling the approach of pain so intense that it forces him to lie flat in bed until it passes. And about twice a year the crises get bad enough to put him into Children’s Hospital at Montefiore in the Bronx, where he’s been a patient since he was a baby.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
He would very much like his life to change. “Just get back into basketball, start going to school, and doing what I want to do as a kid,” he said in a chat at Montefiore on a sunny June day when his family had brought him in for blood tests. “And not be separated from other people and not be different.”
Nathan might soon have that chance. For the first time in the 114 years since sickle cell was originally described in a medical journal—although it existed, undefined, for millennia before then—therapies may end a disease that afflicts 100,000 Americans and millions more throughout the world. Last December the U.S. Food and Drug Administration approved two gene-editing treatments that compensate for the mutated DNA that causes sickling. In clinical trials, most patients who received the treatments had no pain episodes afterward, an indication their cells had ceased to sickle. In the wake of that success, several other gene therapies are moving through clinical trials, and Nathan is joining one.
Once he begins treatment this January in Nashville, Tenn., Nathan will face a grueling year of multiple procedures, including months of isolation in a hospital. But if the treatment succeeds, it will remake his life—and his family’s. For Melissa, her fiancé and Nathan’s two siblings, his illness has been a constant worry. “I got the call a few days after he was born,” Melissa says. “I’m looking at this perfectly healthy child, and it just took all my happiness away in that instant. And from there I’ve had him in a bubble. So this will kind of ease me off of him a bit.”
The approved new therapies and the ones likely to come after them hold the potential to alter the entire experience of sickle cell—and, some advocates hope, to change the way medicine treats people with many other conditions. Sickle cell history includes triumphant breakthroughs in science: Research on the illness signaled the dawn of the era of molecular medicine. Progress in testing and treatment involved dogged work by physicians who would not give up on their patients. Disseminating awareness of risk required ferocious activism by communities. Yet for more than 100 years medical research and practice have also illustrated the costs of racial disregard and a lack of commitment to disadvantaged communities. At the start of the second century of sickle cell science, all those factors will determine what the future of medicine may be.
At its simplest, sickle cell disease is a problem caused by the smallest unit in genetics: a change in a single nucleotide—one of about three billion in the human genome—within a gene that directs the production of one part of hemoglobin, the protein that carries oxygen molecules through the blood. Hundreds of millions of hemoglobin molecules are packed into each red blood cell. The hemoglobin produced by the genetic variant can change shape as it gives up the oxygen it is transporting. That shift forces the enclosing cell to deform and turn rigid, taking on the sickled appearance that gives the disease its name. The distorted cells lodge in blood vessels instead of slipping smoothly through them as round red blood cells do.
The nucleotide substitution in the HBB gene—producing what’s known as hemoglobin S, in contrast to normal hemoglobin A—is heritable. Someone who receives one altered gene from one parent is at risk of sickle cell trait, a condition in which few red blood cells are affected. Someone who receives two copies of the gene—a one-in-four chance if both parents carry it—will have the disease. That leaves them at risk for pain crises, anemia as the stiffened cells break down, organ damage because sickled cells carry less oxygen to tissues, a dangerous blockage of blood vessels in the lungs called acute chest syndrome, high blood pressure, and stroke.
Researchers working in western Africa have traced accounts of sickle cell crises back hundreds of years, noting that the symptoms had specific names in different languages and were understood to occur in generations of families. Sickled cells have been identified in modern studies of mummified tissue from Egypt dating to 3200 B.C.E. and skeletons from Kuwait that were buried in about 200 B.C.E. Scientists at the National Human Genome Research Institute, part of the National Institutes of Health, used a family-tree analysis of almost 3,000 genomes to estimate that the sickle cell mutation first arose in the Sahara approximately 7,300 years ago and was subsequently carried through the African continent by migrations.
At the time that mutation appeared, the Sahara was not a desert; it was green and wet, containing grasslands and forests and permanent lakes, along with the animal and insect life suited to those ecosystems. A type of malaria parasite has been identified in fossils that date back at least 20 million years, and the disease has been infecting humanity from our first emergence. And that seems to be a reason the mutation spread: A single copy of the gene—effectively, having sickle cell trait—conferred protection against severe malaria. It would have been a formidable advantage for people living in some of the most malarious places on the planet. This dynamic offers an explanation for why the sickle cell mutation persisted in sub-Saharan Africa, which still has the highest prevalence of sickle cell disease, and spread around the Mediterranean and into the Middle East.
Different strains of malaria arrived in South America, the Caribbean and the U.S. South in the 1600s. The disease devastated indentured European laborers and enslaved Native Americans. The observation that some African people—kidnapped and then enslaved in the New World—were protected from the worst effects of malaria was perceived as extra incentive for their captivity. Apologists for slavery argued it proved that Africans were intended by nature to be agricultural laborers. Economist Elena Esposito of the University of Lausanne in Switzerland has shown, using sale records incorporating places of origin, that planters paid a premium for enslaved Africans whom they assumed possessed resistance to the disease.
Although there have been many waves of migration from Africa and the Mediterranean to the U.S., historians say much of the sickle cell disease in people of African heritage in the Americas may be traced to the enslavement and transport of their ancestors. The link between sickle cell and a forcibly disadvantaged group set the pattern for how U.S. society would respond to the disease.
The modern study of sickle cell disease began with a descendant of that African diaspora after an unusual set of circumstances allowed him to bypass medicine’s racial segregation. During the 1904 Christmas holidays a dental student in Chicago named Walter Clement Noel sought help for what felt like pneumonia. Noel was Black, but he was not a member of the post–Civil War Great Migration into northern cities. He was a member of an affluent family on the Caribbean island of Grenada and was studying at the Chicago College of Dental Surgery. Benefits available through that post made medical care affordable at four downtown hospitals that Noel otherwise would have been unlikely to approach for care. He crossed the street from his lodgings to what is now Rush University Medical Center and was treated by faculty physician James Herrick and his intern, Ernest Irons.
The two men did a thorough exam of Noel, noting a cough, fever, swollen lymph nodes, a slight heart murmur, and scars on his legs from recurrent ulcers. Nothing notable showed up in a urinalysis, but Irons noticed something odd about Noel’s red blood cells under a microscope. When Herrick described Noel’s case in a medical journal in 1910, he wrote that the blood contained “a large number of thin, elongated, sickle-shaped and crescent-shaped forms.”
“I don’t want to have sickle cell. I would jump through 18 hoops. But jumping through those hoops means risks.”
—Melissa Creary University of Michigan School of Public Health
Noel stayed in the hospital for a month, receiving nourishing food and iron supplements but never a diagnosis. “We were at a loss to account for this peculiar complexus of symptoms,” Herrick admitted in his write-up. The two doctors saw him a number of times until he graduated from dental school in 1907, and then they lost track of him. (They might never have known that he died in Grenada in 1916, ostensibly from pneumonia but probably from complications of sickle cell.) Three other patients with the same symptoms were reported in the next 12 years, in Virginia, Maryland and Missouri. But in 1923 physicians began to recognize the disease in dozens of people. In 1924 American medicine agreed that the constellation of disordered cells, symptoms and family history represented a unique disease rather than the effects of any known pathogen.
There would, of course, have been many more patients than those—but during this period the medical workforce most would have consulted was being eliminated. In 1910, the same year Herrick published his report on Noel, a so-called reform plan for U.S. medical education forced the closure of all but two historically Black medical schools, almost wiping out training for Black physicians because medical schools were otherwise largely segregated. That pushed Black people’s participation in the medical workforce far below their representation in the population. The imbalance has persisted: in 2022 fewer than 6 percent of physicians in the U.S. identified as Black, although more than 13 percent of the population chose that identity in 2020 census data. Researchers say those closed schools would have trained several generations of Black physicians and mentors, an estimated 35,000 missing from the field.
“At the same time that you have this new disease being described, the workforce to take care of [patients] plummets,” says James Taylor VI, director of the Center for Sickle Cell Disease at Howard University. The center at this prominent historically Black university is the oldest one in the U.S. The limits on Black people working as physicians and in other health-care roles, he says, are “the root of so many of the disparities we still see today.”
Restricting Black participation in the medical profession deprived sickle cell patients of health-care workers who would have best understood their needs and may have contributed to the maligning of people experiencing sickling crises as addicts faking pain to obtain opioids. It also might have enabled an enduring pattern in sickle cell research: biochemical discovery racing far ahead of improved patient care.
Chemist Linus Pauling, later a two-time winner of the Nobel Prize, identified the hemoglobin defect in 1949. Once he identified the cause of sickle cell as a mutant hemoglobin molecule, Pauling dubbed sickle cell anemia a “molecular disease.” That framing effectively launched the biomedical era of newly powerful laboratory research. Mark T. Gladwin, a longtime sickle cell researcher who is dean of the University of Maryland School of Medicine, says “sickle cell disease has always led the cutting edge of science discovery, whether it’s understanding the regulation of [genetic] promoter sequences or understanding protein biochemistry and folding. The concepts behind prion disease and amyloidosis, protein-folding diseases, those were predicted by sickle polymerization.”
One of the first drugs to meaningfully help patients was not a novel antisickling agent. Instead it was penicillin, which became available in U.S. pharmacies in 1945. Sickling makes children more vulnerable to a variety of infections, but when child mortality was already high, deaths associated with sickle cell did not stand out from other childhood illness. Antibiotics made it possible to cure those infections, and by preventing death, they allowed the disease to be perceived in survivors. (Twice-daily doses of antibiotics are still routinely prescribed for children younger than five years who have sickle cell disease.)
The first drug that actually made an impact on the disease process of sickle cell was a compound called hydroxyurea. It was originally a cancer drug, but researchers showed it could also prompt production of a type of hemoglobin that is present before birth and in infants but fades after a few months of life. Cells with this kind of hemoglobin resist sickling—an explanation for why newborns with the illness do not experience sickle crises. Hydroxyurea reduces sickle crises and hospitalization by half. Yet it was not tested against the disease or approved by the FDA until the 1990s, nearly 50 years after Pauling’s discovery of the sickle cell mutation.
The dearth of treatments created a kind of feedback loop. Sickle cell looked like a disease in which no progress could be made; because of that, new researchers were discouraged from entering the field, which delayed progress further. Vivien Sheehan, a hematologist and associate professor of pediatrics at Emory University School of Medicine, who leads a lab studying the genomics of sickle cell, recalls an esteemed faculty member telling her during her training not to pursue sickle cell as a career. “I can picture what he thought,” she says. “We had one old drug; there was no pharma interest, no gene therapy. NIH funding was low compared with other genetic diseases.”
What changed the picture was activism. In 1970 a physician named Robert B. Scott, Jr., was a faculty member at what was then a predominantly white medical institution that later became part of Virginia Commonwealth University. That year he wrote a blistering editorial in the Journal of the American Medical Association. He laid out how little funding sickle cell was receiving either from the government or from private donors compared with other genetic diseases. As an example, he estimated that research into cystic fibrosis, which occurred in one out of 2,940 children, received 65 NIH grants in 1968; sickle cell, affecting one in 500 children, received 22. And, highlighting the lack of generational wealth in the Black community, he also estimated that muscular dystrophy research benefited from $7.2 million in volunteer contributions, compared with just $50,000 for sickle cell, which had no national advocacy organization.
Scott did not say explicitly that race was the reason sickle cell had been neglected, but the conclusion was obvious. The following year the Black Panther Party announced it was making sickle cell one of its main priorities, creating a People’s Sickle Cell Anemia Research Foundation and launching a massive educational campaign that included community events offering free screening for sickle cell trait and disease. To put both the editorial and the campaign into context: The Civil Rights Act had passed in 1964, and Martin Luther King, Jr., was assassinated in 1968. A national election was looming in 1972. Maybe to heal the nation—or maybe, more cynically, to attract Black votes—President Richard M. Nixon proposed a sickle cell research program. The National Sickle Cell Anemia Control Act passed in 1972, committing the NIH to creating 10 research and training centers around the country. But crucially, the bill allowed no new money for the effort; instead it was funded by other NIH programs’ budgets. So within several years sickle cell research was back to depending on the energy of individual researchers.
To be clear, these efforts produced life-saving results. In 1997 researchers established that periodic transfusions could reduce the risk of stroke in children diagnosed with sickle cell. In 2007 researchers in France demonstrated that children with sickle cell could be cured with a bone marrow transplant from a donor who was an exact immunological match, such as a full sibling. In 2009 investigators in the U.S. established that a similar process could cure adults. A burst of innovation in the past decade brought three new drugs into sickle cell care: l-glutamine, approved in 2017, and crizanlizumab and voxelotor, both approved in 2019. But researchers say uptake of these new agents has been slow. And hydroxyurea, still the best drug, faces a major usage hurdle: it is contraindicated for pregnant people, based on animal studies and limited human data showing it can produce birth defects.
Sickle cell experts hope more treatments and cures are coming. “What we currently have approved for drug therapies is not adequate,” says hematologist Modupe Idowu, medical director of the UT Physicians Comprehensive Adult Sickle Cell Center in Houston, which treats about 1,300 adults with sickle cell disease. “Hydroxyurea remains the gold standard, but some patients really have reservations about it. Patients must stay on these indefinitely, and they are not curative. And patients continue to have pain episodes, and they continue to have complications.”
Until now, the only true cure for sickle cell has been a bone marrow transplant from a family member who is a perfect immunological match. But only a few patients—between 10 and 20 percent—can identify one. The seemingly benign therapy of periodic transfusions carries its own risks, including a toxic overload of iron that has to be scavenged from the body. And over time excruciating sickling crises rewire pain pathways in the body, leaving patients with chronic pain.
The new gene therapies are an extraordinary scientific achievement, but they are difficult to obtain. The two recent treatments, Casgevy and Lyfgenia, became two of the most expensive drugs on the U.S. market when they were approved, costing $2.2 million and $3.1 million, respectively. Those prices cover only the gene editing of a patient’s own cells—“not the coverage of the hospital stays, or all their visits with me, or the transfusions they will need in preparation, or the central line they will need placed, or the fertility preservation they may want first,” says Kerry Morrone, an assistant professor at Albert Einstein College of Medicine in New York City and director of the sickle cell program treating Nathan at Children’s Hospital at Montefiore. (The clinical trial Nathan has entered will pay for his care.) Approval, in other words, may not equal access and may not meaningfully improve the lives of most people with the disease today.
The gene therapies are built on the back of a stem cell transplant. A patient must receive transfusions to force down the number of sickled cells in their bloodstream, then growth factors to make sure they produce enough new stem cells; they need other drugs to move the cells out from their bone marrow. The stem cells are harvested in a procedure resembling an extended blood draw and sent to the drug companies for genetic editing. Once they are returned, the patient undergoes therapy to kill their disordered cells before the edited ones are infused. The entire process can take a year.
The length, complexity and expense can prompt deep uncertainty in people living with sickle cell disease. Melissa Creary is one of them. She is a social scientist at the University of Michigan School of Public Health who studies the ways science, culture and policy intersect in sickle cell. She is also a sickle cell patient, having been diagnosed at three years old, and for much of her life she experienced few complications. Then, six years ago, when she was 40, an unexpected complication turned her mild case extreme, inflicting severe pain crises and requiring a strict schedule of doctors’ appointments every five weeks, as well as a complex medication regimen.
“I do not ever miss one of these appointments,” Creary says. “I know what the schedule looks like almost a year in advance. I have my community signed up for who’s going to be my buddy because I’m kind of worthless for that day.”
She is considering gene therapy. “I’m having conversations with my providers, people I know personally, people I know professionally,” she says. Her mother wants to see her cured. Yet Creary’s clinician colleagues urged her to wait. Creary cannot be sure what consequences the treatment might have for her career, finances and support network. If an adult treatment program is not set up in Michigan, she would have to be hospitalized in another state.
“I don’t want to have sickle cell anymore, either, despite the ways in which it has literally crafted who I am as a person, as a scholar,” Creary says. “If I could be untethered to the health-care system through gene therapy, I would jump through 18 hoops. But jumping through those hoops also means all kinds of risks, known and unknown.”
Creary advises various groups on equity and antiracism in medicine, and she is also thinking about how the promise and uncertainties of the new therapies will be communicated to other patients. People with sickle cell come into contact with medicine when they are experiencing the worst pain of their lives, she points out; they may act out because of that or have difficulty expressing themselves. They are likely to encounter racism not only in the outside world but within medicine as well, making it challenging to navigate care and to have their concerns taken seriously. And now they may be confronting the possibility that a functional cure could be out of reach for them because of decisions made by insurance companies or by politicians refusing Medicaid expansion plans.
“At the end of the day, this is about trust and mistrust,” Creary says. “We haven’t done what we need to do in order to build the trust with this population, in order for the science to be as efficacious as it needs to be.”
Sickle cell medicine now has two goals. One is to imagine the next genetic therapies, perhaps developing gene edits that can be inserted into a patient without disrupting their immune system and blood cells first. The other, even more important, is to envision fair, thorough and accessible care. Patients and researchers agree that is what’s most essential now.
Historian Keith Wailoo, a professor of history and public affairs at Princeton University and author of several books on sickle cell, says there has been an ongoing mismatch between what medicine has prioritized and what patients need. He co-chaired a committee at the National Academies of Sciences, Engineering, and Medicine that, in 2023, published a report on whether equity can be a required part of innovation. “The core question was, Is it possible to have a society where equitable access to innovation is more than just an afterthought?” he says. “The moment that we’re in right now should be an object lesson for how we need to innovate in a smarter way.”
Across the U.S., medical centers that have transplant programs are evaluating whether they can deliver the new therapies. They also are scrutinizing who might pay for the procedures and associated care because the cost is beyond the reach of most families, and no one knows how insurance companies will respond.
The Centers for Medicare and Medicaid Services are currently negotiating to set prices; after that, state governments would have to opt in. The limitations of medical insurance are not a new story to Americans, but in this case, whether a patient is eligible for these therapies may depend on not just their age and the state of their disease but where they live.
Clinicians and patients did not have discussions about these things in the past, because the concept of transforming the disease was out of reach. But they are having them now. “Before this time, our conversations about disparities have been about making sure patients with sickle cell are getting clinical care,” says Seethal A. Jacob, director of the pediatric sickle cell program at Indiana University and Riley Children’s Health in Indianapolis, which is applying to offer gene therapy. “But now we need to talk about how we close the gap of disparities in access to these treatments.”
Sickle cell medicine has reached a potentially transformative moment. The history of sickle cell is a tale of bravery and agony, effort and neglect, that mirrors the history of the Black experience in America. If these new therapies and the ones that come after them prove truly successful, individual lives will be completely changed. And perhaps a long-standing wound of inequity and injustice might begin to be healed.